Should you treat a fever? It helps to understand how a fever actually works.
Credit: WakeMed.org
It seems counterintuitive that you’d get the shivers when you come down with a fever. You’re hot, but you’re cold? It makes no sense — until you take a look under the hood.
Your body’s thermostat
Our bodies come with a built-in thermostat in the brain’s hypothalamus that’s normally set to around 98 °F. If your body dips below this “set point” —let’s say you wear a tank top in a snowstorm — your brain will turn on a bunch of bodily functions to create and retain heat. That’s why you shiver. Involuntary rapid muscle micro-movements generate heat all over your body. On the flip side, if you overheat — you’re wearing that same tank top at high noon in Black Rock Desert — your brain turns on your sweat glands so that liquid evaporating off of your skin cools you down. This all happens automagically, and your brain is really good at keeping your body’s temperature stable.
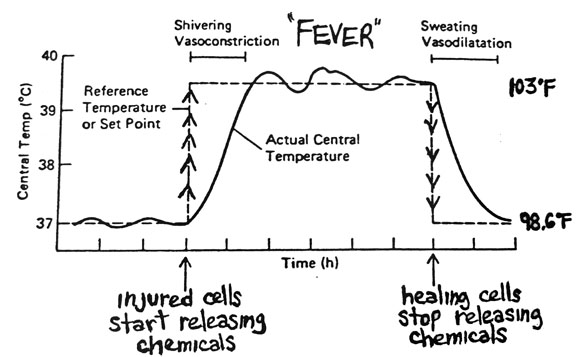
So what’s going on when you get a fever? Fever is a sign of inflammation in your body. An inflammatory response can be triggered by infection, such as a flu virus, or by immune-related diseases, cancer, or even drugs and alcohol. Certain chemicals released during inflammation turn up your body’s thermostat. How high depends on the specific inflammatory response. Technically, a fever is anything above 100.4 °F or 38 °C.
If you come down with an infection, your thermostat resets to, let’s say, 102 degrees, but your body’s still hanging at 98. Your brain thinks your body is too cold, so you involuntarily shiver to warm up. This is how you can have a fever and feel warm on the outside — 101 degrees, on your way to 102 — but get the chills and feel cold inside. Once you warm all the way up to your new set point you’ll feel warm to the touch, but inside, your body will feel just right and you’ll stop shivering.
What about when a fever “breaks”? Let’s say your body has fought off the bug and your inflammatory response is calming down. The thermostat in your hypothalamus resets back to 98 degrees, but now your body temperature is way up at 102. Your brain sends blood to dilated capillaries near the surface of your skin to release heat, and you sweat and wake up in drenched bedsheets. All of this cools you back down to normal body temperature.
Badass graph showing the physiology of a fever from Antranik.org. “Vasoconstriction” is tightened blood vessels, and “vasodilation” is dilated blood vessels.
The thermostat hypothesis explains how fever medications work. Acetaminophen, aspirin, and anti-inflammatory pain relievers like ibuprofen are fever reducers (technically called antipyretics). Among other effects, they inhibit your body’s production of prostaglandins, the chemicals that turn up the thermostat in your brain. During a fever, taking one of these medications will turn your thermostat down a notch or two.
The benefits of fevers
First, the bad: fevers are metabolically expensive. They put stress on your body. Your heart beats faster, you consume oxygen more quickly, your cells consume more energy than usual. Very high temperatures (above 105 °F) can directly damage cells.
Now for the good: despite their metabolic costs, fevers turn up consistently across species as a response to infection, indicating an evolutionary advantage.
A higher body temperature creates an inhospitable environment for many invading bugs to grow and replicate. For example, high temperatures reduce iron levels in the blood, and this makes it hard for bacteria to reproduce. Fevers also appear to boost the immune system to fight off infection. In short, you feel like crap, but you’re actually in a stronger position to beat the bug.
Life in the Fast Lane, a medical blog written by experts in emergency medicine and critical care, cites some fascinating studies from the early 1900s on inducing fevers to cure infections (for obvious ethical reasons, we’d never be able to do this today):
- One study induced fever in patients with neurosyphilis-related muscle paralysis by inoculating them with malaria, treatable with quinine. Remission rates were 30%, compared to 1% spontaneous remission without fever treatment. Incidentally, this “fever therapy” work led to a Nobel Prize in 1927.
- Later, fever therapy — in one case, inducing hyperthermia to 107 °F for six hours in a chamber — led to cure in 81% of gonorrhea cases. And must have been miserable.
A 2013 article on fevers from NYU’s Clinical Correlations cites several lab animal studies showing that “morbidity and mortality decrease when fever is allowed to run its course.” In one study, “infected iguanas that actively raised their body temperatures by moving into warm light survived the infections, whereas individuals that were prevented from seeking a warm environment grew sicker and died.” In other words, even cold-blooded animals that can’t internally regulate their temperature move to a warm rock when they get sick.
In humans, a randomized ICU study at the University of Miami was stopped because patients treated “aggressively” (for any temperature above 101.3 degrees) had a significantly higher mortality rate than patients treated “permissively” (only when their body temperature went above 104 degrees). That said, several similar studies cited by Life in the Fastlane showed no significant difference in mortality between patients given fever reducers versus placebo treatment.
On a population level, there’s even evidence that suppressing fevers with antipyretics leads to increased transmission of the flu virus and, therefore, more cases of the flu and flu-related deaths.
So should you treat a fever?
A fever is a sign of infection, but it may also be part of its cure.
The idea that any fever must be treated immediately with medication could be wrong in many cases. Fever reducers treat a sign, not the cause, of your illness, and lowering your temperature may get in the way of your body’s normal defenses — for example, prolonging flu symptoms by hindering your body’s ability to fight off the virus.
Here’s when doctors worry: When a fever is very high (above 105 °F), prolonged, in an infant, or in a critically ill patient. Otherwise, a fever on its own isn’t dangerous, and there’s no real need to treat it.
Doctors also worry about dehydration with fevers, especially if there’s associated vomiting or diarrhea. If a child urinates less than three times or an infant has fewer than three wet diapers in 24 hours, she’s already dehydrated and should be seen by a doctor immediately. The most important thing to remember with a fever is to stay hydrated. It’s okay if you don’t feel much like eating (that’s a normal, even adaptive, response), but keep drinking water. Kids can drink Pedialyte, too.
Another reason doctors worry tends to have less to do with the number on your thermometer and more to do with how you look and feel. If your child has a fever and is lethargic (so sleepy you can’t wake her) or inconsolable (can’t stop crying), take her to a doctor right away. If you technically have a fever but feel okay, or your child has a fever but she’s still playing, eating, and drinking, doctors don’t worry. If your child has a fever and seems fussy, she’s probably uncomfortable, just as many of us are when we’re sick — it’s no fun — but she’s not seriously ill. It’s your choice to treat a low to moderate fever in yourself or your child to alleviate discomfort, but there’s no medical need to treat the fever itself. (For kids, use children’s acetaminophen or ibuprofen. Don’t give aspirin to children under 18.)
When to see a doctor right away for a fever
- Fever above 100.4 °F in an infant under 3 months old
- Fever above 102.2 °F in an infant 3–12 months old
- Fever in an unvaccinated child
- Very high fever (above 105 °F)
- Fever lasting longer than 48–72 hours
- Fever plus other serious symptoms such as shortness of breath, abdominal pain, headache that doesn’t go away with over-the-counter pain medication, neck stiffness, redness or swelling in joints or arms and legs, coughing up blood, bloody diarrhea, recent unexplained weight loss, or unusual fatigue that doesn’t go away
- Fever in an IV drug user
- Fever in someone with a serious illness (like cancer) or immunosuppression (like HIV)
Read more about fevers and when to contact a medical professional on MedlinePlus. In my opinion it’s the best-written health info online. Bookmark it!
-----
A version of this article was originally published on Iodine.com.